For decades, Body Mass Index (BMI)" >Body Mass Index (BMI) has been the go-to measurement for assessing weight status and related health risks. Doctors, fitness professionals, and insurance companies all rely on this simple calculation to categorize individuals as underweight, normal weight, overweight, or obese. However, growing evidence suggests that BMI has significant limitations and may not provide an accurate picture of a person's health or body composition. This article explores the shortcomings of BMI and introduces five alternative measurements that offer more comprehensive health assessments.
What is BMI and How is it Calculated?
Body Mass Index was developed in the 1830s by Belgian mathematician Adolphe Quetelet as a simple way to assess weight in relation to height. The formula divides a person's weight in kilograms by the square of their height in meters:
BMI = weight (kg) / [height (m)]²
For those using imperial measurements, the formula is:
BMI = [weight (lbs) × 703] / [height (inches)]²
According to standard BMI categories:
- Below 18.5: Underweight
- 18.5 to 24.9: Normal weight
- 25.0 to 29.9: Overweight
- 30.0 and above: Obese (with further subdivisions for higher BMI values)
BMI gained widespread adoption because it's easy to calculate, requires minimal equipment (just a scale and height measurement), and provides a standardized way to classify weight status across populations. Despite its simplicity and convenience, however, BMI has several critical limitations that affect its accuracy and usefulness.
The Limitations of BMI
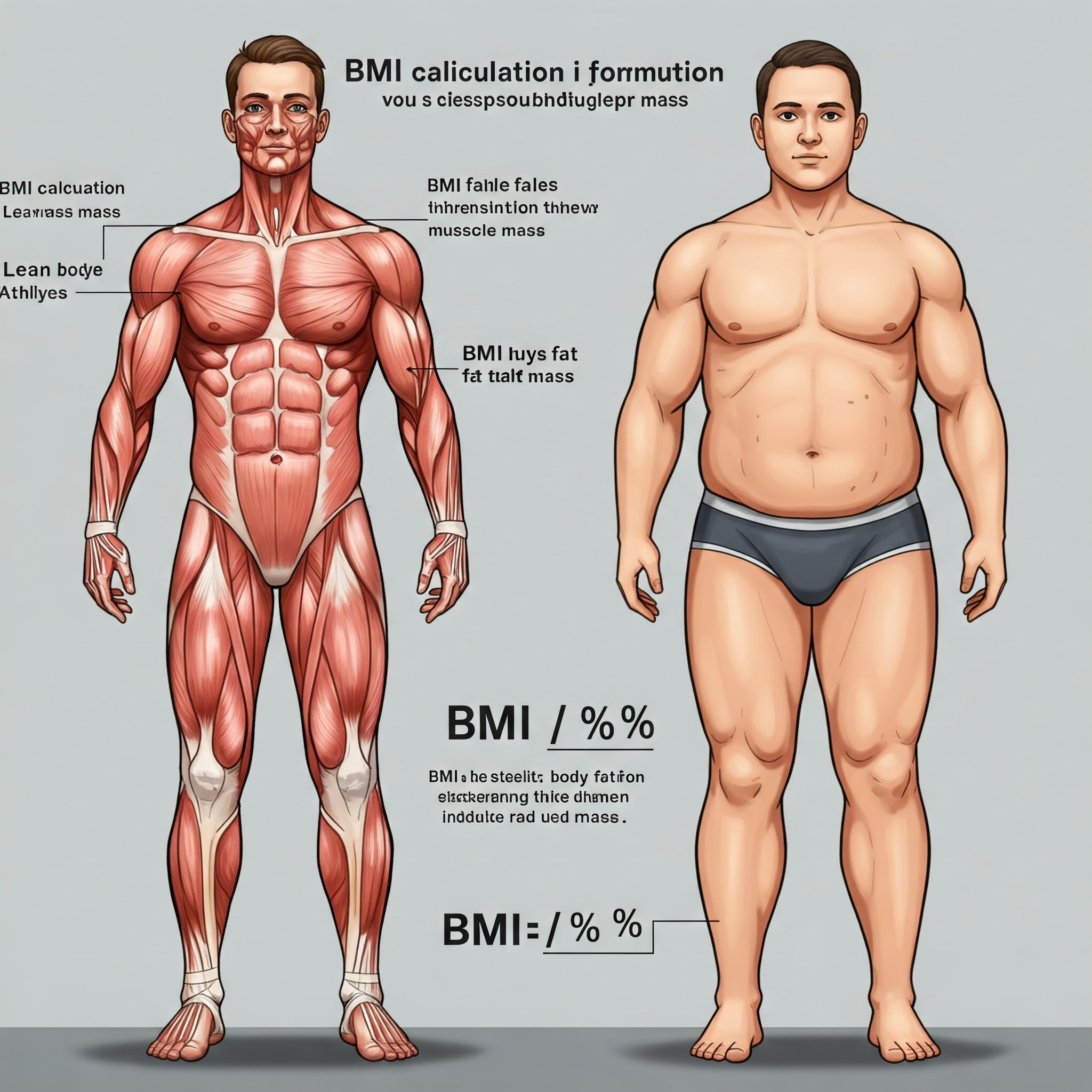
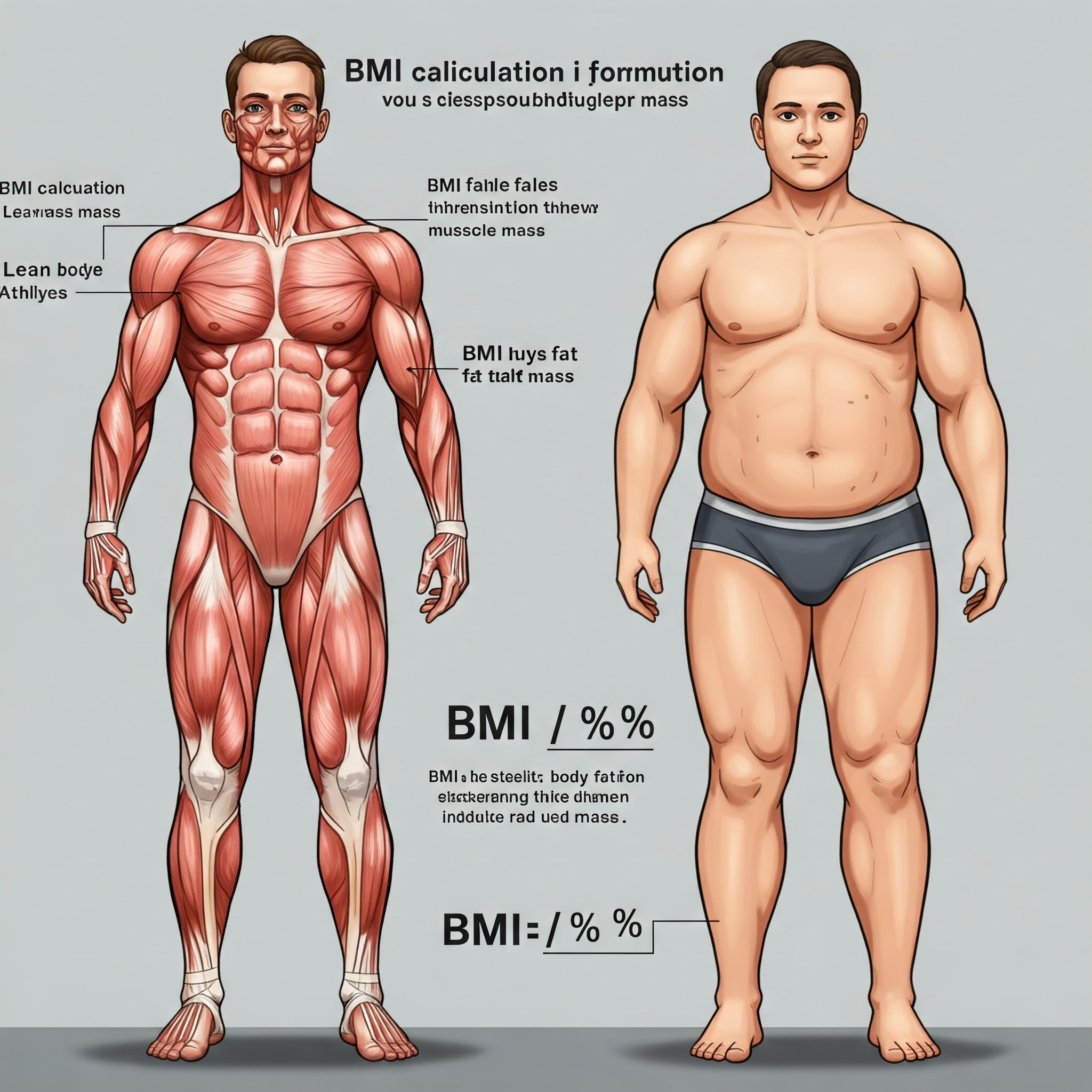
1. Doesn't Distinguish Between Fat, Muscle, and Bone
Perhaps the most significant limitation of BMI is that it only considers total body weight relative to height, without differentiating between different tissues. A muscular athlete with very low body fat might be classified as overweight or obese according to BMI, despite being in excellent physical condition. Muscle tissue is denser than fat, meaning that two people with identical heights and weights can have dramatically different body compositions and health profiles.
This limitation is particularly problematic for:
- Athletes and bodybuilders
- People who engage in regular strength training
- Individuals with naturally dense bone structure
2. Ignores Fat Distribution and Location
Not all body fat carries the same health risks. Research has consistently shown that visceral fat (fat stored around the abdominal organs) poses significantly greater health risks than subcutaneous fat (fat stored under the skin, particularly around the hips and thighs). BMI makes no distinction between different types of fat or where it's stored in the body.
Someone with an "apple-shaped" body (carrying excess weight around the abdomen) typically faces higher risks for conditions like heart disease and type 2 diabetes than someone with a "pear-shaped" body (carrying excess weight around the hips and thighs), even if they have identical BMI values.
3. Doesn't Account for Age, Sex, or Ethnicity
BMI applies the same standards across all demographics, but body composition naturally varies based on age, sex, and ethnicity:
- Age: Muscle mass tends to decrease and fat percentage increases with age, even if weight remains stable. An older adult might have a "normal" BMI but unhealthy body fat levels.
- Sex: Women naturally have higher body fat percentages than men. A healthy body fat range for women is about 21-33%, compared to 8-19% for men.
- Ethnicity: Different ethnic groups have different body compositions. For example, people of Asian descent typically have more body fat at lower BMI values than people of European descent, leading some health organizations to recommend lower BMI cutoffs for certain populations.
4. Oversimplifies Complex Health Relationships
BMI categories create artificial cutoff points that don't necessarily reflect health risks accurately. The difference between a BMI of 24.9 (classified as "normal") and 25.0 (classified as "overweight") is negligible, yet these values place individuals in different risk categories. Health risks generally increase along a continuum rather than suddenly changing at specific BMI thresholds.
5. Developed Based on Limited Population Data
Quetelet developed BMI based on data from European men in the 19th century. The formula was not designed with diverse populations in mind, and its application to women, children, older adults, and non-European populations may not be appropriate.
Given these limitations, health professionals increasingly recognize the need for alternative measurements that provide more comprehensive assessments of body composition and health risks.
Five Alternative Measurements for More Comprehensive Health Assessment
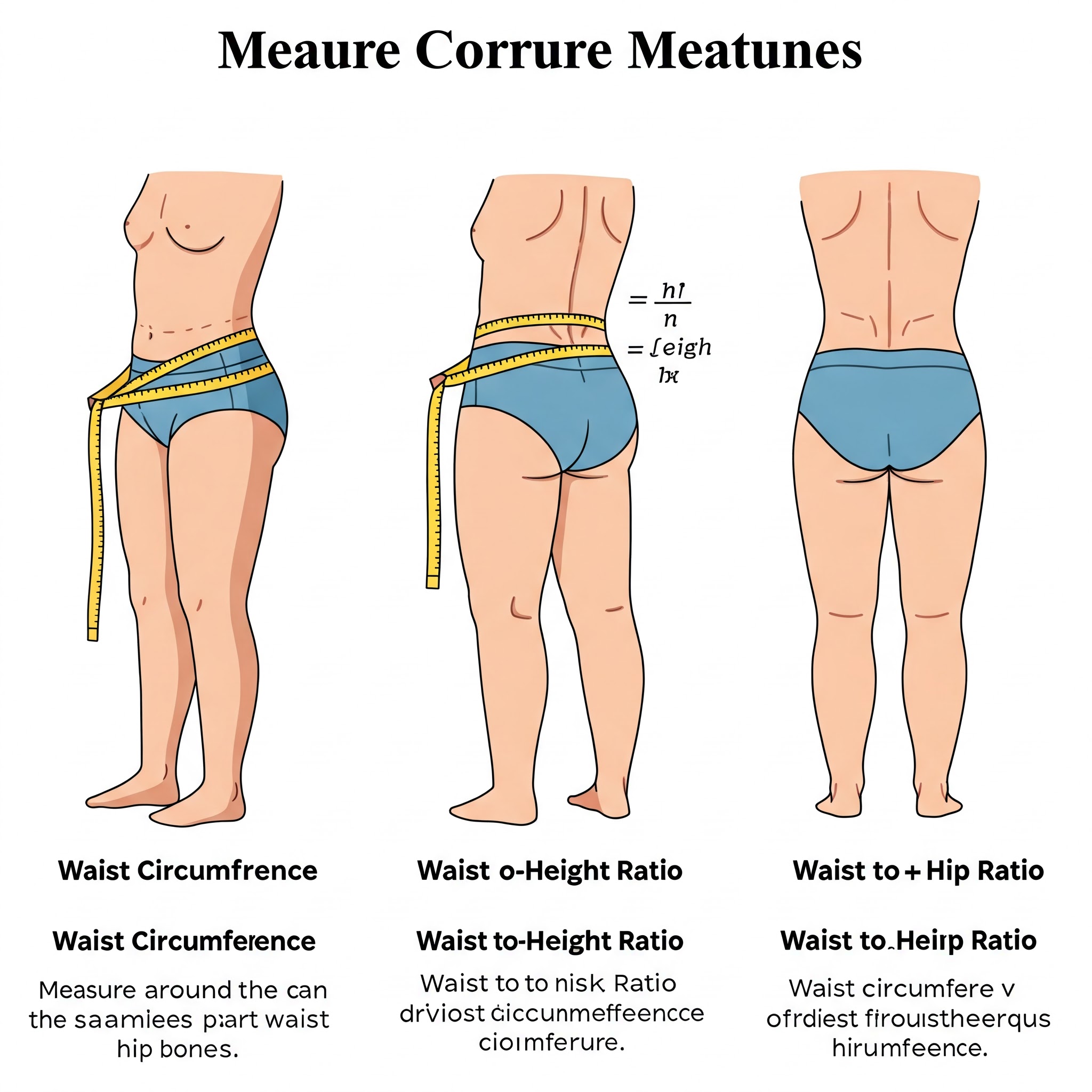
1. Waist Circumference (WC)
Waist circumference directly measures abdominal fat, which is strongly associated with health risks including heart disease, type 2 diabetes, and metabolic syndrome. This simple measurement requires only a tape measure and can be performed at home.
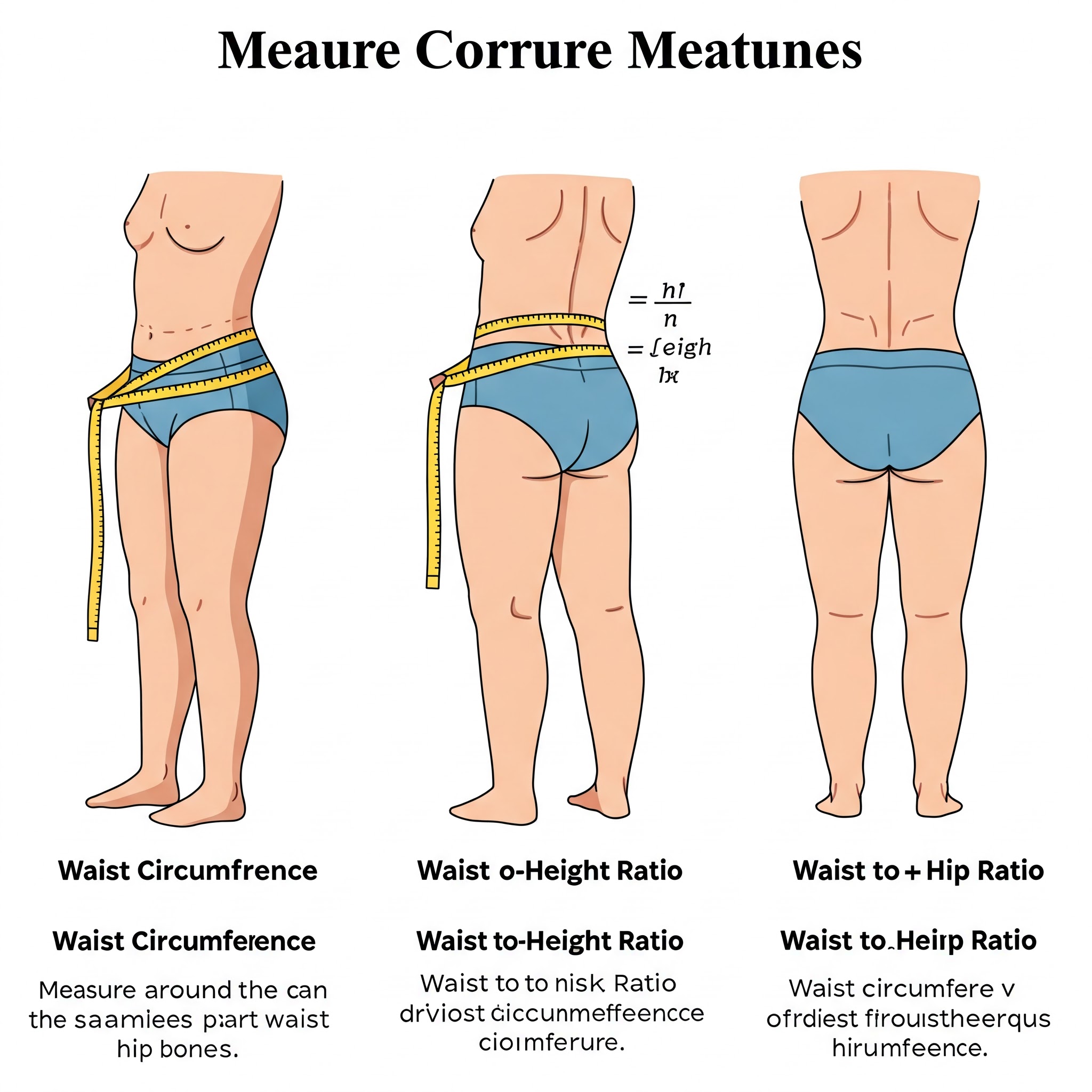
How to measure waist circumference:
- Stand upright with feet shoulder-width apart
- Find the midpoint between the bottom of your ribs and the top of your hip bones
- Wrap a tape measure around your waist at this point
- Take the measurement after exhaling normally, without sucking in your stomach or pulling the tape too tight
Health risk thresholds:
- For men: Increased risk at > 40 inches (102 cm)
- For women: Increased risk at > 35 inches (88 cm)
- These thresholds may be lower for Asian populations (> 35 inches for men, > 31 inches for women)
Advantages:
- Simple, inexpensive, and can be done at home
- Directly measures abdominal fat, a key health risk indicator
- Better predictor of cardiovascular disease risk than BMI alone
Limitations:
- Doesn't account for overall body composition
- May be less accurate for very tall or very short individuals
- Measurement technique can vary, affecting consistency
Waist circumference is especially valuable when combined with BMI, as the two measurements together provide a more complete picture than either one alone.
2. Waist-to-Height Ratio (WHtR)
The waist-to-height ratio addresses some limitations of waist circumference alone by accounting for a person's height. This is particularly useful because taller people naturally tend to have larger waists even if they have healthy body fat levels.
How to calculate WHtR:
- Measure your waist circumference (as described above)
- Divide this measurement by your height (using the same units)
- WHtR = Waist circumference ÷ Height
Health risk thresholds:
- WHtR < 0.5: Lower health risk ("Keep your waist circumference less than half your height")
- WHtR ≥ 0.5: Increased health risk
- WHtR ≥ 0.6: Substantially increased health risk
Advantages:
- Accounts for both abdominal fat and height
- Easy to calculate and remember (aim for less than half your height)
- Studies suggest it may be the best single predictor of cardiovascular risk and mortality
- Applies fairly consistently across different age groups, sexes, and ethnicities
Limitations:
- Still doesn't measure overall body composition
- May not be as accurate for growing children or those with certain body shapes
Recent research has shown that WHtR may be more reliable than both BMI and waist circumference alone, particularly in identifying health risks in normal-weight individuals who carry excess abdominal fat.
3. Waist-to-Hip Ratio (WHR)
Waist-to-hip ratio compares the circumference of the waist to that of the hips, providing information about body fat distribution patterns. This ratio helps distinguish between "apple" and "pear" body shapes, which carry different health implications.
How to calculate WHR:
- Measure your waist circumference
- Measure your hip circumference (at the widest part of your buttocks)
- Divide the waist measurement by the hip measurement
- WHR = Waist circumference ÷ Hip circumference
Health risk thresholds:
- For men: Increased risk at WHR > 0.90
- For women: Increased risk at WHR > 0.85
Advantages:
- Assesses body fat distribution pattern
- Strong predictor of heart disease and type 2 diabetes risk
- Helps identify health risks that BMI might miss
- Validated across multiple population studies
Limitations:
- More complex to measure accurately than waist circumference alone
- Hip measurement can be affected by bone structure
- Two people with different amounts of total body fat could have the same WHR
WHR is particularly valuable for identifying individuals with normal BMI but unhealthy fat distribution patterns, who might otherwise be categorized as "healthy" by standard metrics.
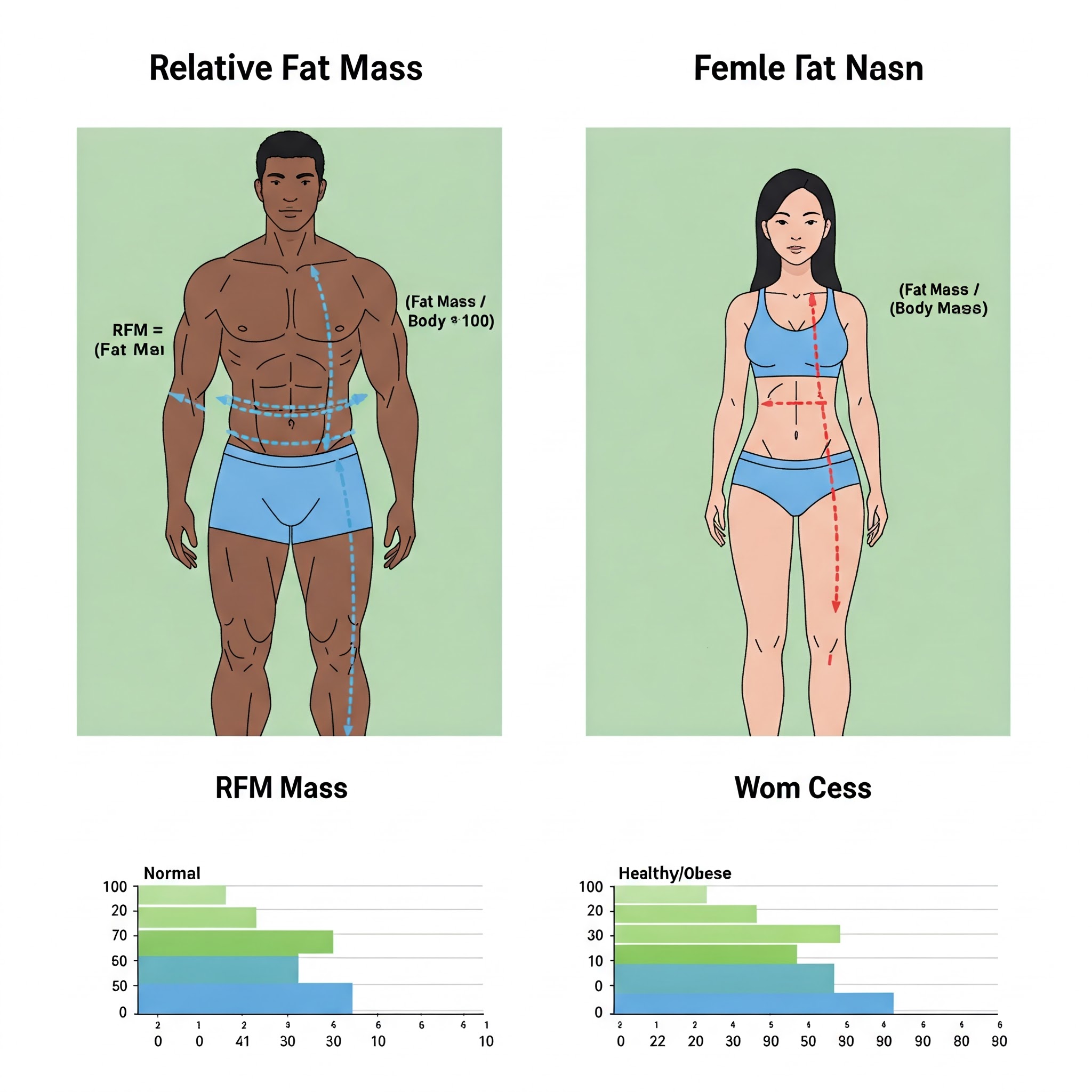
4. Relative Fat Mass (RFM)
Relative Fat Mass is a newer measurement developed in 2018 by researchers at Cedars-Sinai Medical Center. It was specifically designed to provide a more accurate estimate of body fat percentage than BMI, while still being simple enough to calculate without specialized equipment.
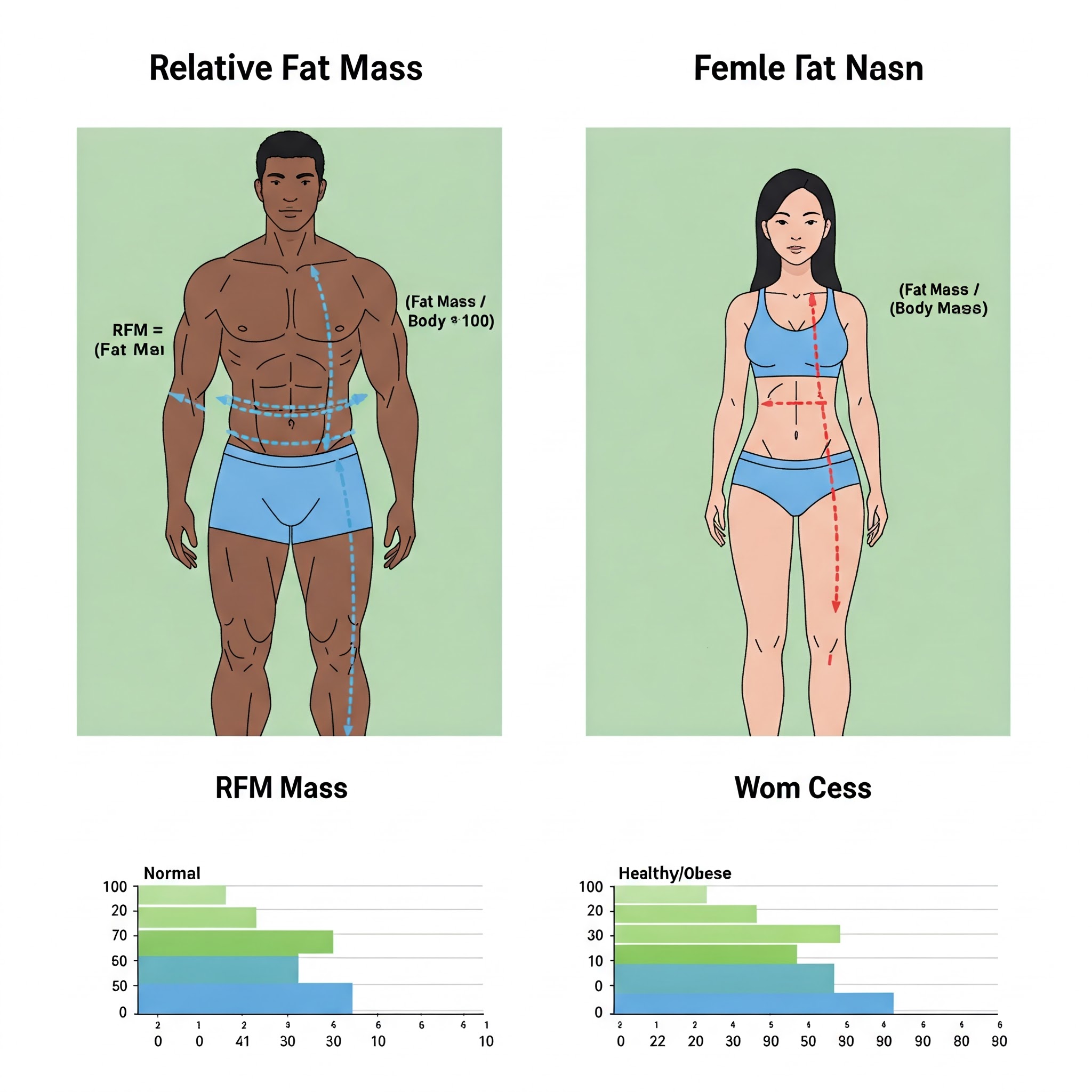
How to calculate RFM:
- For men: RFM = 64 – (20 × height/waist circumference)
- For women: RFM = 76 – (20 × height/waist circumference)
- (Height and waist circumference must be measured in the same units)
Health risk thresholds:
- For men: Body fat > 25% indicates increased risk
- For women: Body fat > 35% indicates increased risk
Advantages:
- Better correlation with actual body fat percentage than BMI
- Requires only a tape measure, no scale needed
- Accounts for sex differences with separate formulas
- Simple enough for home use or clinical settings
Limitations:
- Relatively new, with fewer long-term studies than other measurements
- Doesn't account for differences in muscle mass between individuals
- May not be as accurate for extreme body types
RFM represents an important advancement in accessible body composition assessment, offering improved accuracy over BMI without requiring sophisticated technology.
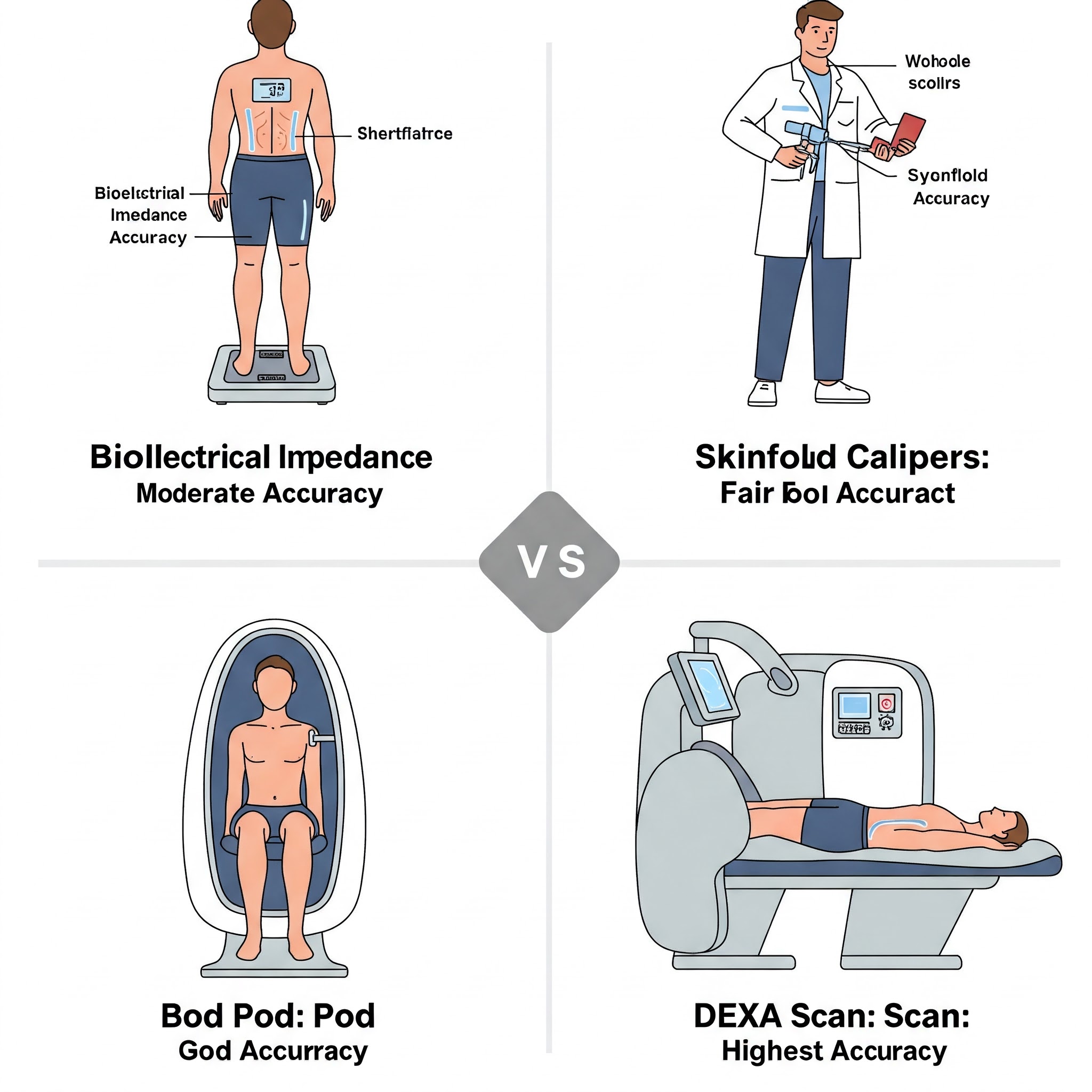
5. Body Fat Percentage Methods
For the most comprehensive assessment of body composition, directly measuring body fat percentage provides valuable information that BMI and other ratio-based methods cannot. Several methods exist for estimating body fat percentage, with varying levels of accuracy, convenience, and cost.
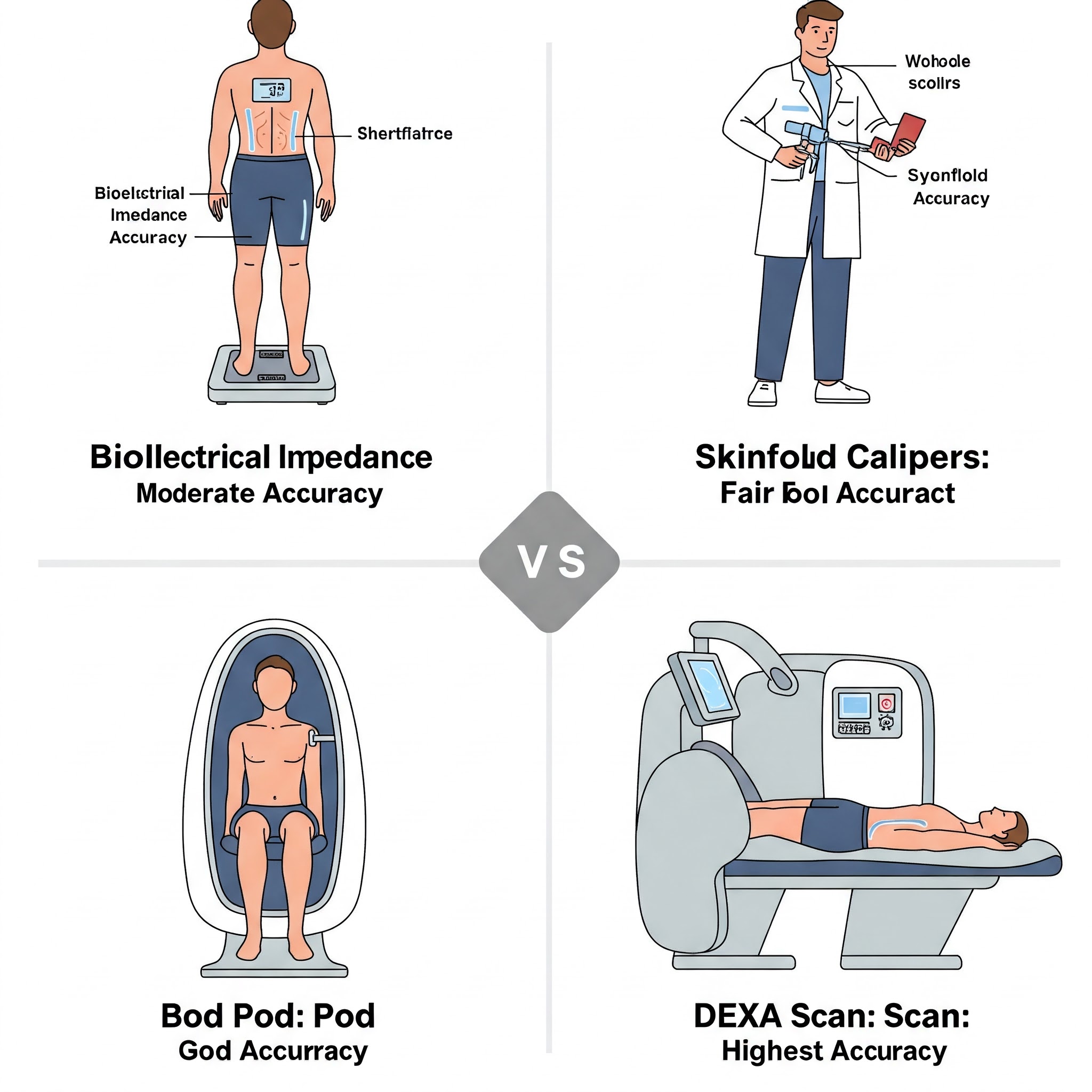
Bioelectrical Impedance Analysis (BIA):
- Uses a weak electrical current passed through the body
- Based on the principle that fat conducts electricity differently than muscle and water
- Available in consumer scales, handheld devices, and professional equipment
- Accuracy can be affected by hydration level, recent exercise, and food intake
- Generally accurate within 3-5% of more advanced methods when quality equipment is used
Skinfold Measurements:
- Uses calipers to measure the thickness of skin folds at multiple body sites
- Measurements are used in formulas to estimate overall body fat percentage
- Requires trained personnel for accurate measurements
- Relatively inexpensive but requires proper technique
- Can be less accurate for very lean or obese individuals
Air Displacement Plethysmography (Bod Pod):
- Measures the air displacement caused by the body in a sealed chamber
- Uses this data to calculate body density and estimate fat percentage
- More accurate than BIA or skinfold measurements
- Available at some fitness centers, universities, and medical facilities
- Requires specialized equipment and trained operators
Dual-Energy X-ray Absorptiometry (DEXA):
- Uses low-dose X-rays to measure bone, fat, and lean tissue
- Considered the "gold standard" for body composition assessment
- Provides regional body composition data (trunk, limbs, etc.)
- Requires specialized medical equipment and trained operators
- More expensive than other methods but highly accurate
Underwater Weighing (Hydrostatic Weighing):
- Based on Archimedes' principle that fat floats while muscle sinks
- Involves being weighed underwater after exhaling
- Traditionally considered a reference standard for body composition
- Requires specialized equipment and is less convenient than newer methods
- Still highly accurate when performed correctly
Health risk thresholds for body fat percentage:
- For men: Essential fat (3-5%), Athletic (6-13%), Fitness (14-17%), Acceptable (18-24%), Obese (>25%)
- For women: Essential fat (10-13%), Athletic (14-20%), Fitness (21-24%), Acceptable (25-31%), Obese (>32%)
Advantages:
- Directly measures the component of body composition most relevant to health risks
- Provides more accurate information than weight-based measurements
- Can track changes in body composition during weight loss or fitness programs
- Distinguishes between fat loss and muscle loss
Limitations:
- Most accurate methods require specialized equipment
- Consumer devices (like BIA scales) have variable accuracy
- Results can be affected by hydration, recent exercise, and other factors
- More time-consuming and expensive than simpler measurements
Body fat percentage measurement provides the most comprehensive assessment of body composition but may not be practical for routine monitoring due to cost and accessibility constraints.
Combining Measurements for Comprehensive Assessment
No single measurement provides a complete picture of body composition and health risk. The most comprehensive approach combines multiple measurements to assess different aspects of body composition and fat distribution.
A practical approach for most individuals might include:
- BMI as an initial screening tool
- Waist circumference or WHtR to assess abdominal fat
- Body fat percentage (if accessible) for overall body composition
For healthcare professionals, additional measurements might include:
- Blood pressure
- Cholesterol levels
- Blood glucose
- Physical fitness assessments
- Family history
By looking at multiple indicators rather than relying solely on BMI, individuals can gain a more accurate understanding of their body composition and potential health risks.
Making Sense of Your Measurements
When interpreting these measurements, keep in mind:
- Consistency matters more than absolute numbers. Track changes over time using the same measurement method and technique.
- No single measurement defines health. Consider your measurements alongside other health indicators including physical activity level, diet quality, sleep, stress, and other lifestyle factors.
- Different bodies have different healthy ranges. Age, sex, ethnicity, and individual factors all influence what's healthy for you specifically.
- Body composition is just one aspect of health. Physical fitness, mental wellbeing, and metabolic health are equally important considerations.
- When in doubt, consult a healthcare professional. They can help interpret your measurements in the context of your overall health and specific circumstances.
Conclusion
While BMI has served as a convenient tool for assessing weight status, its limitations highlight the need for more comprehensive measurements. Waist circumference, waist-to-height ratio, waist-to-hip ratio, relative fat mass, and body fat percentage all provide valuable information that BMI alone cannot capture.
By understanding these alternative measurements and how they complement each other, individuals and healthcare providers can make more informed decisions about health risks and interventions. The future of body composition assessment will likely involve multiple measurements, potentially combined with advanced technologies like 3D body scanning, to provide increasingly personalized health insights.
Remember that all these measurements are tools for understanding health risks, not definitive statements about individual health status or worth. They should inform—but never replace—a holistic approach to health that includes physical activity, nutritious eating, adequate sleep, stress management, and other lifestyle factors that contribute to overall wellbeing.
References
- Nuttall, F. Q. (2015). Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutrition Today, 50(3), 117-128. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890841/" target="_blank" rel="nofollow">https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890841/
- Ashwell, M., Gunn, P., & Gibson, S. (2012). Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obesity Reviews, 13(3), 275-286. https://pubmed.ncbi.nlm.nih.gov/22106927/" target="_blank" rel="nofollow">https://pubmed.ncbi.nlm.nih.gov/22106927/
- Woolcott, O. O., & Bergman, R. N. (2018). Relative fat mass (RFM) as a new estimator of whole-body fat percentage ─ A cross-sectional study in American adult individuals. Scientific Reports, 8(1), 10980. https://www.nature.com/articles/s41598-018-29362-1" target="_blank" rel="nofollow">https://www.nature.com/articles/s41598-018-29362-1
- Agbaje, A. O. (2024). Waist-circumference-to-height-ratio had better longitudinal agreement with DEXA-measured fat mass than BMI in 7237 children. Pediatric Research, 96, 1369-1380. https://www.nature.com/articles/s41390-024-03112-8" target="_blank" rel="nofollow">https://www.nature.com/articles/s41390-024-03112-8
- World Health Organization. (2011). Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. https://www.who.int/publications/i/item/9789241501491" target="_blank" rel="nofollow">https://www.who.int/publications/i/item/9789241501491